At Inovalon your continued health is important to us. Our goal is to provide you with meaningful choices to fit your needs while ensuring you have access to quality and affordable care.
Medical Insurance
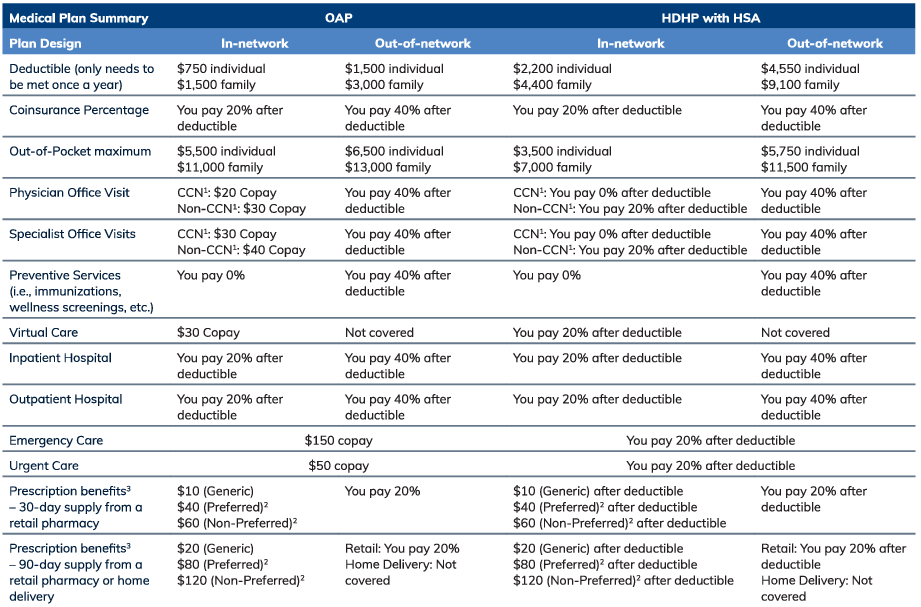
You have two medical plan options through Allegiance utilizing the Cigna Open Access Plus (OAP) network:
- Open Access Plus (OAP)
- High Deductible Health Plan (HDHP) with HSA
Managing Your Medical and Prescription Benefits
Healthcare doesn’t have to be confusing. To make things easier, Inovalon has partnered with Quantum Health to simplify your healthcare experience, get the most out of your benefits, and save you money.
Filing an Out-of-Network Claim with Allegiance
Online: Visit the Allegiance Submit a Claim web page and complete the online form.
By Mail: Download the form and mail to Allegiance.
Allegiance
P.O. Box 3018
Missoula, MT 59806-3018
Need Help?
Quantum Health Care Coordinators are available to help with questions regarding your medical and prescription drug plans. Call Quantum Health at 1-866-885-1125 for all your health care needs.
Get the MyQHealth app
Follow these simple steps to obtain your medical and prescription drug member ID card:
- Open the Apple App Store or Google Play
- Search for “MyQHealth — Care Coordinators”
- Select the app and tap “Install” to begin downloading
- Open the app and register your account
Comparing Your Medical Plan Options
- The Cigna Care Network (CCN) consists of healthcare professionals that are assigned the Cigna Care Designation (CCD), meaning that they meet Cigna’s criteria for certain quality and cost-efficiency measures. The Cigna Care Network (CCN) provides a higher level of in-network benefits (coinsurance and/or copayment), so you pay less when you visit a CCN provider. Visit myinovaloncarecoordinator.com.
- When a generic is available and you request a preferred brand or non-preferred brand drug, you pay the brand cost share plus the cost difference between the brand and generic drugs up to the cost of the brand drug (unless your physician indicates “Dispense as Written”).
- Certain prescriptions that are considered to be preventive under federal law are mandated to be covered in full and the noted cost sharing does not apply. For a list of ACA approved preventive care, go to healthcare.gov.
Additional Details:
Precertification is required for certain services. For a list of services, refer to the back of your ID card.
If you cover any dependents on the HDHP with HSA plan, the full family deductible must be met before the plan will start to pay. The above is a brief summary of the plans. For a more detailed summary, go to www.myinovalonbenefits.com.
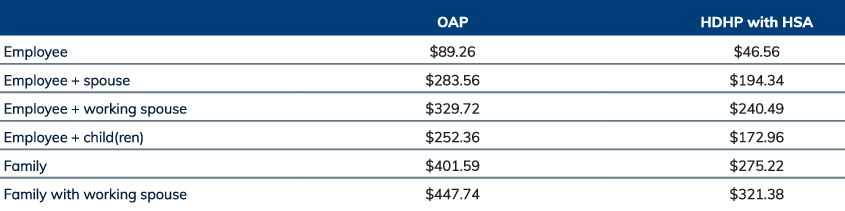
Medical and Prescription Biweekly Payroll Contributions
Prescription Drug Coverage
Inovalon offers a prescription drug plan through Cigna. Each medical plan automatically comes with prescription drug coverage. You will use your medical plan’s ID card to fill prescriptions at one of Cigna’s participating pharmacies. You can fill a 30-day supply at any retail pharmacy in the network, including CVS, Walmart, Publix, and several others. Or, you may fill a 90-day supply at a select in-network retail pharmacy including CVS, Walmart, etc. For a full list of participating chain retail pharmacies, go to Cigna.com, or go to cigna.com/rx90network.